Resources suggested by Dr Pietersen, thankyou. Starting with @KiJinnChin :
This is a simple step-by-step guide to the basic principles of safe and effective axillary brachial plexus blockade. A 2nd video with further tips and tricks is here – https://youtu.be/09tkxrGzoDk 00:07 – Indications 00:32 – Preparation 01:10 – Positioning 01:46 – Scanning phase 02:20 – US anatomy 05:04 – Perivascular injection technique 06:12
Considerable anatomic variation is noted for all the terminal branches of the brachial plexus; however the most common orientations are:
Median Nerve – anterior lateral to the artery (above and slightly left, at the 10 to 12 o’clock position relative to the artery)
Ulnar Nerve – anterior medial to the artery (above and to the right, near the axillary vein, 1-3 o’clock position relative to the artery)
Radial Nerve – posterior medial to the artery (below and to the right, between 3 to 6 o’clock positions relative to the artery)
Musculocutaneous Nerve – optimal imaging requires more lateral positioning of the transducer as it lies within the coracobrachialis muscle or fascia just below the biceps muscle
This image from NYSORA
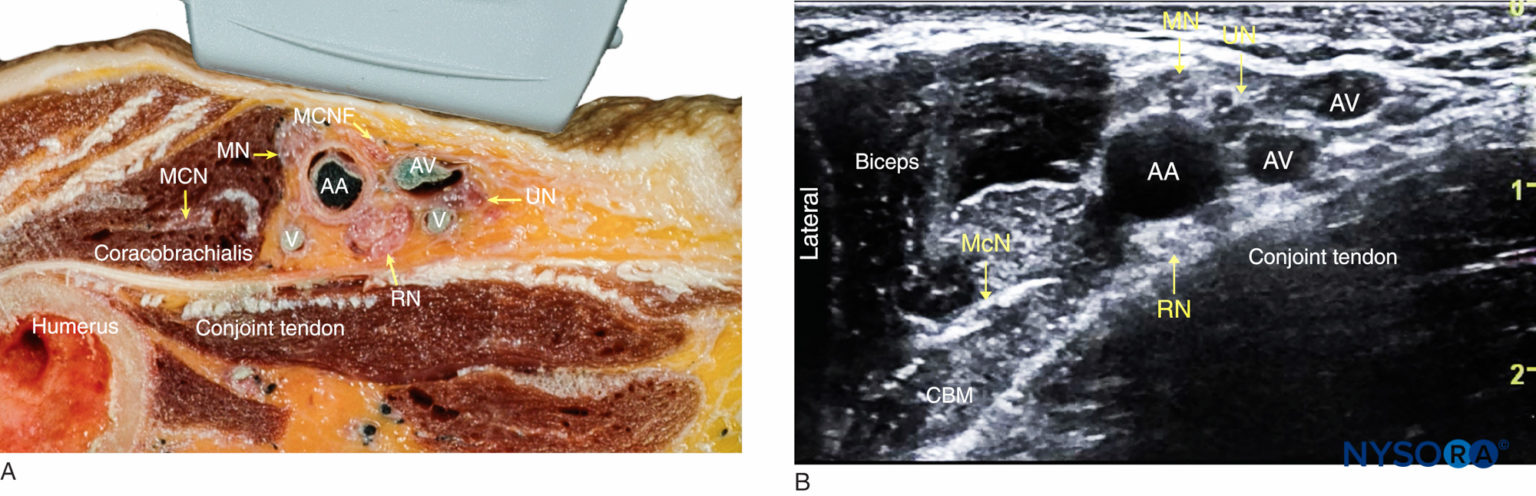 FIGURE 1. (A) Cross-sectional anatomy of the axillary fossa and ultrasound image (B) of the terminal nerves of brachial plexus. The BP is seen scattered around the axillary artery and enclosed within the adipose tissue compartment containing the axillary artery (AA), and axillary veins (AV). MCN, musculocutaneous nerve. MN, median nerve; RN, radial nerve; UN, ulnar nerve; MACN, medial antebrachial cutaneous nerve; CBM, coracobrachialis muscle
FIGURE 1. (A) Cross-sectional anatomy of the axillary fossa and ultrasound image (B) of the terminal nerves of brachial plexus. The BP is seen scattered around the axillary artery and enclosed within the adipose tissue compartment containing the axillary artery (AA), and axillary veins (AV). MCN, musculocutaneous nerve. MN, median nerve; RN, radial nerve; UN, ulnar nerve; MACN, medial antebrachial cutaneous nerve; CBM, coracobrachialis muscle
Supplemental Nerve Blocks
- Musculocutaneous nerve block can be performed by injecting 5-10 mL of local anesthetic into the body of the coracobrachialis muscle in a fanlike manner in a lateral to medial plane. This technique is indicated if the musculocutaneous nerve is not identified by nerve stimulation/ultrasound or if a transarterial approach is used.
- Intercostobrachial and medial brachial cutaneous nerve block helps to prevent tourniquet-related pain because the intercostobrachial nerve (T2) joins the medial brachial cutaneous nerve to innervate the skin of the upper half of the medial and posterior part of the arm. At the site of needle insertion, 5-8 mL of local anesthetic is injected subcutaneously across the axilla both superior and inferior to the artery. The intercostobrachial nerve may be seen on ultrasound imaging, and does not always need a separate supplemental block if performed proximal enough or viewed on ultrasound.
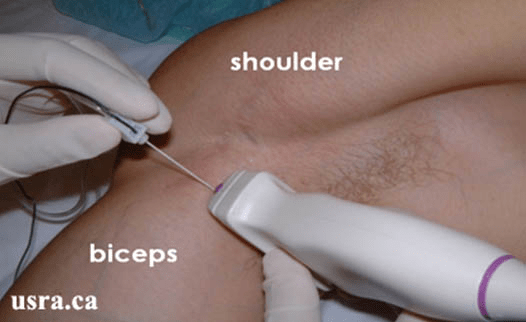
This from USRA.CA
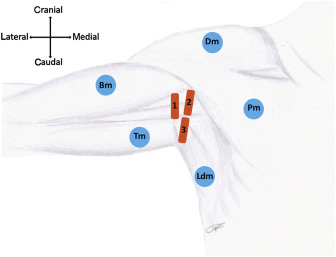
This from the BJA in 2018

Leave a comment